Contents
- 📏 Recommended Amounts of Sodium
- 🧂 Types of Salt: How Much Sodium Are You Really Getting?
- 🩺 Sodium and Your Health: Why Too Much Can Hurt
- ❤️ Salt and Heart Health: What the Science Really Shows
- 🧠 Salt and Chronic Kidney Disease: What’s the Connection?
- 🍽️ Food Sources of Sodium: Where It’s Really Coming From
- 🧂 Are “Natural” Salts Healthier Than Table Salt?
- ⚠️ Signs of Deficiency and Toxicity
- 🧬 The Interplay of Sodium and Potassium
Sodium is essential to life, but balance is key. It helps regulate blood pressure and volume, supports muscle function (including the heart), and maintains fluid balance in and around cells. However, when sodium intake consistently exceeds the body’s needs, it can have harmful effects — especially on the cardiovascular system.
When there is too much sodium in the bloodstream, it pulls water into the blood vessels, increasing the total volume of blood. This, in turn, raises blood pressure. Over time, high blood pressure (hypertension) puts strain on the heart, arteries, kidneys, and brain. This can lead to a higher risk of heart attack, stroke, kidney disease, and cognitive decline.
Excess sodium may also increase calcium excretion in urine. Over the long term, this may reduce bone mineral density, especially in people who consume too little calcium. This is one way sodium could indirectly contribute to osteoporosis.
In summary, while sodium is crucial in small amounts, too much can silently harm the body over time — especially when combined with a diet low in fruits, vegetables, and whole grains, which help counterbalance sodium’s effects.
📏 Recommended Amounts of Sodium
Unlike many nutrients, sodium does not have an established Recommended Dietary Allowance (RDA) or Tolerable Upper Intake Level (UL) due to limited evidence on deficiency or toxicity at specific levels—outside of its well-documented link to chronic diseases. However, two key intake benchmarks have been defined:
- Adequate Intake (AI):
For adults and teens aged 14 and older—including pregnant women—the AI is 1,500 mg of sodium per day. This is based on the lowest sodium levels shown in controlled studies to support normal body function without signs of deficiency. - Chronic Disease Risk Reduction (CDRR) Intake:
To reduce the risk of chronic conditions like high blood pressure and cardiovascular disease, the CDRR threshold is 2,300 mg per day. Staying below this level is associated with meaningful health benefits for the general population.
Despite these guidelines, most Americans consume around 3,400 mg of sodium daily—well above both the AI and CDRR targets. The excess typically comes not from the salt shaker, but from packaged, processed, and restaurant foods, where sodium is often hidden.
🧂 Types of Salt: How Much Sodium Are You Really Getting?
Not all salt is created equal. The texture and density of different types of salt influence how much sodium they deliver per teaspoon. Finely ground salts are denser and typically pack more sodium than coarse crystals. Sodium content can also vary by brand, so it’s always best to check the Nutrition Facts label.
Here’s a comparison of common salts and their approximate sodium content per teaspoon:
| Salt Type | Sodium (mg/teaspoon) |
|---|---|
| Iodized Table Salt, fine | 2,300 mg |
| Kosher Salt, coarse | 1,920 mg |
| Kosher Salt, fine (Diamond Crystal®) | 1,120 mg |
| Sea Salt, fine | 2,120 mg |
| Sea Salt, coarse | 1,560 mg |
| Pink (Himalayan) Salt | 2,200 mg |
| Black Salt | 1,150–2,200 mg |
| Fleur de Sel | 1,560–2,320 mg |
| Potassium Salt (Salt Substitute) | 0 mg sodium (2,760–3,180 mg potassium) |
📝 Note: Brand names like Diamond Crystal® are included for reference only and do not imply endorsement.
🩺 Sodium and Your Health: Why Too Much Can Hurt
When we consume too much sodium, our kidneys struggle to keep up. As sodium builds up in the bloodstream, the body retains water to dilute it. This extra water increases:
- 💧 Fluid around cells
- 💓 Blood volume
The result? More work for your heart and increased pressure on blood vessels, which can lead to:
- High blood pressure (hypertension)
- Heart disease and heart failure
- Stroke
- Kidney damage
- Stiffened arteries (arteriosclerosis)
- Bone loss (due to calcium leaching from bones)
Some research even shows that excess salt can harm the heart, aorta, and kidneys independently of its effect on blood pressure.
🔎 Want to dive deeper? Learn more about specific health risks linked to high sodium intake in the sections below.
❤️ Salt and Heart Health: What the Science Really Shows
Too much sodium in the diet is a major contributor to high blood pressure, which in turn is a leading risk factor for cardiovascular disease (CVD). High blood pressure causes:
- 2 out of 3 strokes
- 1 out of 2 heart disease deaths
- Over 1 million preventable deaths per year in countries like China
Even though reducing sodium lowers blood pressure, the link between sodium and CVD outcomes like heart attack or stroke has shown mixed results in research—but the overall trend supports sodium reduction.
🧬 Genetics and Salt Sensitivity
People don’t respond to salt the same way. Some are “salt-sensitive” and benefit more from sodium reduction. These groups tend to respond best:
- Adults over 50
- African-Americans
- Women
- People with high starting blood pressure
📊 Key Studies That Show the Impact of Sodium on Heart Health
🔬 Intersalt Study
- Studied 10,000+ adults in 32 countries.
- Higher sodium intake = higher blood pressure with age.
- People consuming <1,300 mg sodium/day had low blood pressure across all ages.
🧪 TOHP (Trials of Hypertension Prevention)
- Long-term follow-up showed:
- 25% lower risk of heart attack, stroke, or CVD death with sodium reduction.
- Best results in people with a high potassium-to-sodium intake ratio.
📉 TOHP Follow-Up (2000)
- Those consuming <2,300 mg/day had a 32% lower risk of CVD compared to high-sodium consumers (3,600–4,800 mg/day).
🥗 DASH Diet Studies
- Emphasizing fruits, vegetables, and low-fat dairy lowered blood pressure.
- Combining DASH with low-sodium intake had the strongest blood pressure-lowering effect.
📚 Meta-Analysis & Urine Studies
- A review of multiple clinical trials showed that reducing sodium to ~4,000 mg/day decreased blood pressure in all groups (regardless of race or baseline BP).
- Harvard researchers using 24-hour urine samples found:
- For each 1,000 mg increase in sodium, CVD risk went up by 18%
- For each 1,000 mg increase in potassium, CVD risk dropped by 18%
- High sodium-to-potassium ratios = higher risk of heart events
🧠 Key Takeaway: Even small reductions in sodium, especially when combined with higher potassium intake (from fruits, veggies, legumes, and dairy), can significantly lower your risk of cardiovascular disease.
🧠 Salt and Chronic Kidney Disease: What’s the Connection?
Chronic kidney disease (CKD) and cardiovascular disease are closely linked—and high blood pressure is a major shared risk factor. People with CKD are often more salt-sensitive due to their reduced ability to excrete sodium, which can raise blood pressure and worsen kidney function.
🔬 What Does the Research Say?
- Very high sodium intake (>4,600 mg/day) is linked with faster progression of CKD.
- Low sodium intake (<2,300 mg/day) has no clear benefit compared to moderate intake (2,300–4,600 mg/day) in improving CKD outcomes.
- Current research doesn’t strongly support aggressive low-sodium restriction in CKD patients.
✅ Recommended Sodium Guidelines for CKD Management
- <4,000 mg/day for general CKD management
- <3,000 mg/day for those with:
- Fluid retention
- Proteinuria (excess protein in urine, a marker of kidney damage)
🧂 Bottom line: A moderate sodium intake is considered safest and most effective for people with CKD—especially to help control blood pressure and reduce the risk of further kidney damage.
🦴 Salt and Osteoporosis: A Hidden Risk for Your Bones
Most people associate salt with high blood pressure—but too much sodium may also weaken your bones. How? By increasing the amount of calcium lost in urine. If your blood is low in calcium, your body may pull calcium from bones, weakening them over time.
🧪 What the Research Shows
- A study in postmenopausal women found that higher sodium excretion was strongly linked to hip bone density loss—just as strongly as low calcium intake.
- Other research suggests that lowering salt intake improves calcium balance, helping to slow bone loss with age.
📉 Why It Matters
- Excess sodium = more calcium loss
- More calcium loss = greater osteoporosis risk
- Especially important for older adults and postmenopausal women
🧂 Bottom line: Reducing sodium intake not only protects your heart but may also help preserve bone strength as you age.
🍽️ Food Sources of Sodium: Where It’s Really Coming From
Sodium is everywhere—whether you add it or not. Unlike nutrients we seek out, sodium tends to sneak into our diets through processed and prepared foods. In fact, over 70% of sodium intake in the average diet comes from packaged and restaurant foods, not the salt shaker.
🥦 Naturally Low-Sodium Foods
Unprocessed and minimally processed foods are naturally low in sodium:
- Fresh fruits and vegetables
- Whole grains (like oats, brown rice, quinoa)
- Unsalted nuts and seeds
- Fresh meats, poultry, and fish
- Plain dairy products like milk and yogurt
These foods are naturally nutrient-dense and contribute to a healthy eating pattern without excess sodium.
🧂 Top 10 Hidden Sodium Sources (According to the CDC)
You might be surprised where most of the salt in your diet is hiding:
- Breads and rolls
- Pizza
- Sandwiches (especially with cold cuts or cheese)
- Cold cuts and cured meats (e.g., ham, bacon, salami)
- Soups
- Burritos and tacos
- Savory snacks (chips, pretzels, crackers)
- Chicken (especially pre-seasoned or breaded)
- Cheese
- Eggs and omelets (particularly when prepared in restaurants)
🔍 Tip: Check food labels and choose low- or reduced-sodium versions when available—especially in breads, sauces, soups, and ready-to-eat meals.
🧂 Are “Natural” Salts Healthier Than Table Salt?
Many people reach for sea salt or Himalayan pink salt believing they’re healthier than regular table salt. But are they really? The truth: all salts are primarily sodium chloride, and the differences in health impact are minimal.
🔍 Nutritional Differences Are Small
- All salts—table, sea, kosher, pink—contain roughly the same amount of sodium by weight.
- Some natural salts (like sea salt and pink salt) may contain trace minerals like potassium, magnesium, calcium, or iron.
- However, these minerals exist in such tiny amounts that they offer no meaningful nutritional benefit.
🧂 Table Salt
- Source: Mined and highly refined.
- Additives: Iodine (to prevent deficiency), anticaking agents (e.g., calcium silicate).
- Use: Versatile and ideal for baking due to its fine grain and consistent flavor.
✡️ Kosher Salt
- Texture: Coarse flakes.
- Additives: Typically no iodine; may contain anticaking agents.
- Best for: Seasoning meat and vegetables; not interchangeable 1:1 with table salt due to size.
🌊 Sea Salt
- Source: Evaporated seawater.
- Minerals: May include small traces of zinc, potassium, or iron.
- Caution: May contain trace ocean contaminants like lead.
- Flavor: Milder, crunchy texture, great for finishing dishes.
🏔️ Himalayan Pink Salt
- Source: Ancient salt mines in Pakistan.
- Color: Pink from iron oxide.
- Minerals: Contains trace amounts of iron, calcium, magnesium.
- Best used: As a finishing salt or visual garnish.
⚖️ Bottom Line
While “natural” salts can add variety in texture and taste, they are not healthier than iodized table salt. If you do not use iodized salt, make sure to get enough iodine from other foods like dairy, seafood, or fortified products.
💡 Cooking Tip: Because coarser salts pack less tightly into a spoon, volume substitutions vary. Always adjust measurements when swapping between salt types.
⚠️ Signs of Deficiency and Toxicity
Understanding sodium imbalance is important, even though true deficiencies are rare. Both too little and too much sodium in the body can have serious health effects.
🧂 Sodium Deficiency (Hyponatremia)
Though rare in the U.S., hyponatremia (low blood sodium levels) can occur, particularly among:
- Older adults in long-term care facilities
- Hospitalized patients on certain medications
- People experiencing heavy fluid losses (vomiting, diarrhea, excessive sweating)
- Individuals with conditions like heart failure or liver cirrhosis
- Athletes or individuals who drink excessive amounts of water without replacing sodium
What happens?
Sodium is diluted by too much fluid or lost through bodily fluids, disrupting nerve and muscle function.
Common symptoms include:
- Nausea and vomiting
- Headaches
- Confusion or altered mental state
- Lethargy or fatigue
- Muscle cramps
- Seizures or coma (in severe cases)
🚨 Sodium Toxicity (Hypernatremia)
Hypernatremia is too much sodium in the blood and usually stems from dehydration rather than overconsumption of salt alone.
At-risk groups include:
- Older adults with cognitive or physical impairments
- People with high fevers, infections, or vomiting/diarrhea
- Individuals taking diuretics or not drinking enough fluids
- People with kidney dysfunction
What happens?
Water leaves the body’s cells to balance sodium levels in the blood, potentially causing cell damage and organ strain.
Symptoms of hypernatremia may include:
- Intense thirst
- Weakness or fatigue
- Confusion or disorientation
- Nausea and vomiting
- Difficulty breathing (from fluid in the lungs)
- Seizures, coma, or death in extreme cases
- Possible kidney damage
⚖️ Balance is key. Most people don’t need to seek out sodium—it’s already abundant in the modern diet. But staying hydrated and moderating intake is essential to avoid health complications.
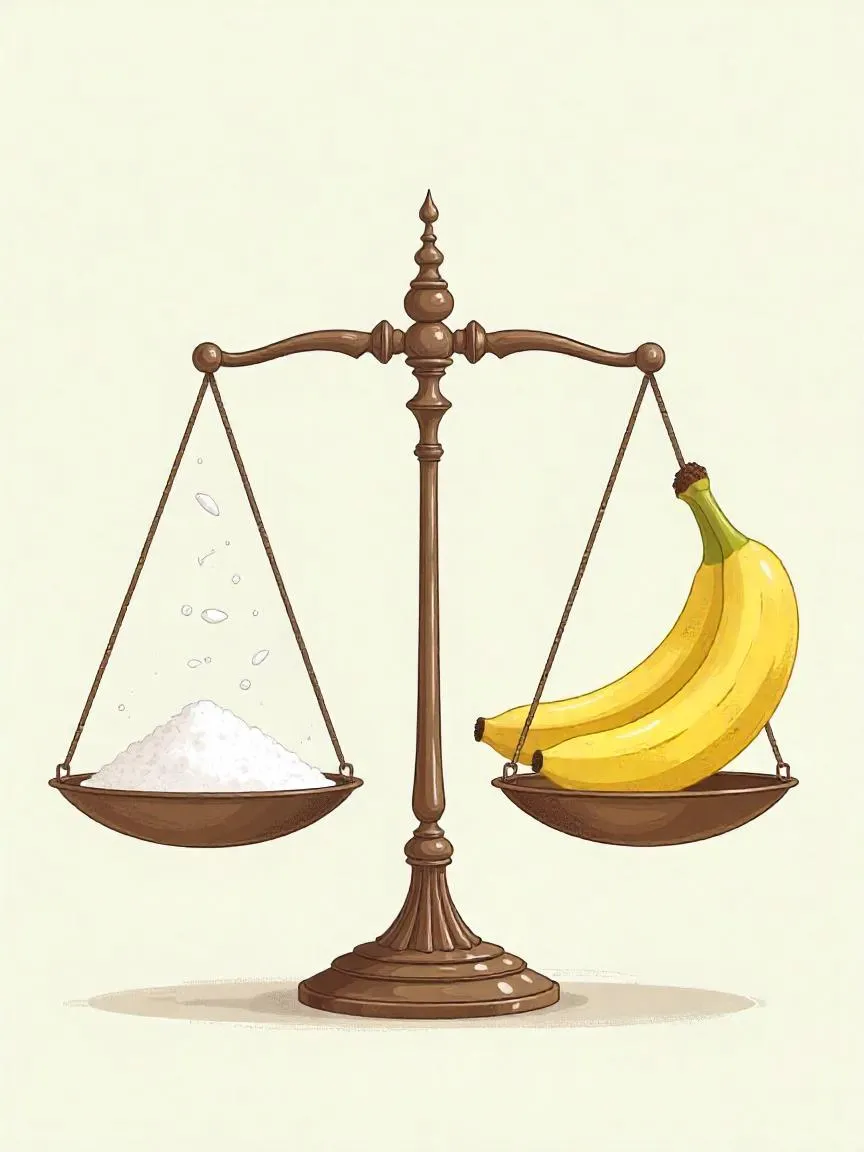
🧬 The Interplay of Sodium and Potassium
Sodium and potassium are essential minerals that work in opposition but in harmony to regulate fluid balance, nerve function, and blood pressure. While both are vital to health, their effects on the body — and on cardiovascular risk — are quite different.
🔄 Opposing Functions, Shared Impact
- Sodium tends to raise blood pressure by causing the body to retain fluid.
- Potassium, on the other hand, helps relax blood vessels and promotes sodium excretion through urine, thereby lowering blood pressure.
An optimal balance between these two nutrients is critical — and most Americans don’t have it.
📊 The Imbalance in the Typical U.S. Diet
- Average sodium intake: ~3,300 mg/day (mainly from processed foods)
- Average potassium intake: ~2,900 mg/day
⚠️ In contrast, our bodies require more potassium than sodium for optimal health — yet the modern diet delivers the reverse.
📚 What the Research Says
A study published in the Archives of Internal Medicine revealed striking findings:
- People with high sodium + low potassium diets had a higher risk of dying from heart attacks and all causes.
- High sodium intake alone was linked to a 20% increased risk of death from any cause.
- High potassium intake was linked to a 20% decreased risk of death.
- The sodium-to-potassium ratio was the most telling:
- Those with the highest ratio had twice the risk of heart attack death.
- They also had a 50% higher risk of death from any cause.
🥦 A Simple Fix with Big Impact
✅ Eat more potassium-rich, whole foods:
- Fresh fruits (bananas, oranges, apricots)
- Vegetables (spinach, sweet potatoes, squash)
- Beans and lentils
- Dairy (yogurt, milk)
- Nuts and seeds
🚫 Cut back on sodium-heavy processed foods:
- Cured meats, cold cuts
- Packaged snacks and instant meals
- Canned soups and processed cheeses
- Breads and sandwich staples
🧠 Remember: It’s not just about lowering sodium — it’s about increasing potassium too. Improving the balance between the two is one of the most effective ways to support heart health and reduce chronic disease risk.










Loving the information on this site, you have done outstanding job on the posts.