Contents
- Why Diet Matters for Cholesterol
- Understanding Cholesterol — Good vs. Bad (LDL vs. HDL)
- Foods That Help Lower LDL (“Bad” Cholesterol)
- Foods to Avoid or Limit for Heart Health
- Role of Fiber — How It Supports Cholesterol Balance
- Healthy Fats vs. Harmful Fats — Choose the Right Oils
- Eat the Rainbow — Fruits, Veggies & Antioxidants
- Sample Daily Meal Plan for Cholesterol Control
- Lifestyle Factors That Complement a Cholesterol-Lowering Diet
- FAQ — What People Really Ask About Diet and Cholesterol
Why Diet Matters for Cholesterol
When most people hear the word cholesterol, they immediately picture lab results, doctor appointments, and long lists of foods to avoid. But the truth is much softer — and much more empowering. Your daily meals have an incredible ability to support your heart, balance cholesterol levels, and gently steer your health in a better direction without extreme diets or complicated rules.
Think of your plate as a quiet partner in your wellbeing. Every time you choose foods rich in fiber, healthy fats, or antioxidants, you’re giving your body tools to lower “bad” LDL cholesterol and strengthen “good” HDL — the type that protects your arteries. And the best part? These changes don’t require harsh restrictions. They often begin with small adjustments that feel natural, comforting, and enjoyable.
Picture this: a warm bowl of oats in the morning topped with berries and nuts, a colorful lunch filled with vegetables and olive oil, a simple dinner featuring salmon and whole grains. These are not “diet foods.” They’re heart-supporting, nourishing meals that help you feel stronger, lighter, and more energized over time.
Cholesterol isn’t the enemy. It’s simply something to be understood — and gently balanced.
And while medication can be helpful for some people, food is your first, most accessible, most deeply effective tool. With the right ingredients, you can improve cholesterol numbers in a matter of weeks and support your cardiovascular health for years to come.
This guide will show you how. We’ll explore what cholesterol really is, which foods help lower unhealthy levels, what to limit, and how to build everyday meals that naturally support your heart. The goal isn’t perfection — it’s small, meaningful steps that fit your life and taste good too.
Ready? Let’s begin with understanding the basics: the difference between “good” and “bad” cholesterol — and why both matter.
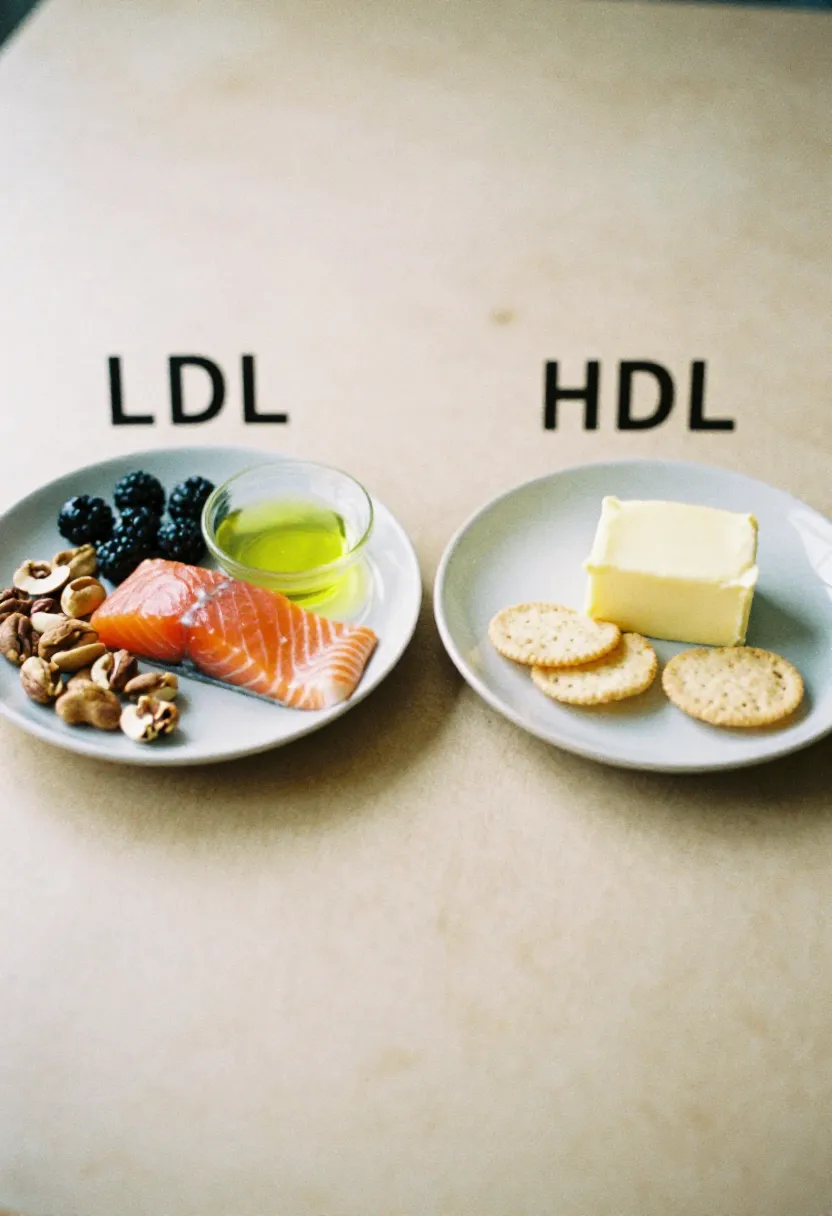
Understanding Cholesterol — Good vs. Bad (LDL vs. HDL)
Before you can lower cholesterol through food, it helps to understand what cholesterol actually is. And surprisingly, it’s not the villain many people imagine. Cholesterol is a waxy, fat-like substance your body needs to build hormones, support cell membranes, and make vitamin D.
The problem isn’t cholesterol itself — it’s imbalance.
There are two main types, and each plays a different role in your health.
LDL — “Bad” Cholesterol (the one to lower)
LDL stands for low-density lipoprotein.
You can think of LDL as the “delivery truck” that carries cholesterol through your bloodstream. When there’s too much LDL, it starts to leave cholesterol on artery walls, like dust collecting in narrow hallways. Over time, this buildup forms plaque — the main risk factor for heart disease and stroke.
High LDL is usually connected with:
- diets high in saturated or trans fats
- low fiber intake
- lack of physical activity
- genetics
When people talk about “lowering cholesterol,” they’re mostly talking about lowering LDL.
HDL — “Good” Cholesterol (the one to raise)
HDL stands for high-density lipoprotein.
HDL works like a cleanup crew — it travels through the bloodstream, picks up excess cholesterol, and carries it back to the liver where it can be broken down or removed.
Higher HDL levels can help:
- protect your arteries
- reduce inflammation
- lower your risk of heart disease
Foods rich in healthy fats and regular physical activity naturally increase HDL.
Triglycerides — The Often-Forgotten Third Piece
While not technically cholesterol, triglycerides are another type of fat in your blood. When triglycerides are high and LDL is high, the combination becomes far more risky.
They’re often elevated due to:
- high sugar intake
- excess alcohol
- overweight or insulin resistance
- refined carbs
- oversized portions
The good news?
The same heart-friendly diet that lowers LDL also reduces triglycerides — a powerful two-in-one effect.
Why Balance Matters More Than “Good” or “Bad”
Some cholesterol is essential.
Some is harmful in excess.
What truly matters is the ratio — how much LDL compared to HDL. A diet rich in fiber, healthy fats, whole foods, and antioxidants helps shift this ratio in your favor.
Understanding these basics makes it easier to see why certain foods help (and others don’t). Next, we’ll look at the most supportive foods for naturally lowering LDL and boosting HDL — the foods your heart will thank you for.
Foods That Help Lower LDL (“Bad” Cholesterol)
Lowering LDL doesn’t have to feel restrictive. In fact, it often begins by adding nourishing, supportive foods to your meals rather than taking things away. Certain ingredients work beautifully with your body to pull cholesterol out of your bloodstream, reduce inflammation, and strengthen your heart.
Here’s a closer look at the foods that naturally help bring LDL down — and why they’re so powerful.
Oats & Whole Grains — Gentle Helpers for Your Heart
Oats are one of the most studied cholesterol-lowering foods in the world, thanks to a special type of soluble fiber called beta-glucan. This fiber forms a gel-like substance in your gut that binds to cholesterol and carries it out of your body.
Whole grains like barley, quinoa, and brown rice offer a similar benefit.
A warm bowl of oatmeal in the morning is one of the simplest and most effective first steps.
Beans & Lentils — Fiber-Rich, Filling, and LDL-Friendly
Beans, chickpeas, and lentils provide a big dose of soluble fiber, plant protein, and slow-burning carbohydrates. They help lower LDL while keeping you full longer — ideal for stabilizing appetite and supporting weight balance (another key factor for cholesterol health).
Even adding beans to soups or salads a few times a week can make a noticeable difference.
Fatty Fish — Omega-3 Power for Your Heart
Salmon, mackerel, sardines, trout, and herring are rich in omega-3 fatty acids, which don’t directly lower LDL but play a big role in reducing triglycerides, calming inflammation, and supporting HDL (the “good” cholesterol).
For heart health, aim for two servings a week.
Nuts & Seeds — Small Foods, Big Impact
Almonds, walnuts, chia seeds, and flaxseeds are full of fiber, healthy fats, and plant sterols — natural compounds that block cholesterol absorption.
A small handful a day is enough to see benefits.
Not a diet — just a delicious habit.
Olive Oil — The Gold Standard of Healthy Fats
Extra-virgin olive oil is rich in monounsaturated fats and antioxidants that have been shown to lower LDL while improving HDL.
It’s one of the simplest swaps you can make:
replace butter with olive oil when possible.
Your heart will feel the difference.
Colorful Fruits & Vegetables — Antioxidants at Work
Fruits and vegetables (especially apples, berries, citrus, carrots, spinach, and broccoli) contain antioxidants that prevent LDL from oxidizing — a key step in plaque formation.
More color on your plate = more heart protection.
Aim for 2–3 colors each meal.
Avocados — Creamy & Heart-Loving
Avocados are rich in monounsaturated fats and fiber, making them a double-strength ally for lowering LDL. They work beautifully in sandwiches, salads, or even as a simple spread.
Dark Chocolate & Cocoa (Yes, Really!)
In moderation, cocoa and dark chocolate (70%+ cacao) contain flavonoids that support heart health and reduce LDL oxidation.
A small square is enough — a delicious, heart-friendly treat.
Why These Foods Work Together
Soluble fiber, plant compounds, and healthy fats create a synergistic effect — they help remove cholesterol from the body, prevent buildup, and support healthy blood vessels. When eaten regularly, they shift your cholesterol levels in a meaningful, lasting way.
Next, we’ll look at the foods you may want to limit — not eliminate — to support the same goals.
Foods to Avoid or Limit for Heart Health
When it comes to managing cholesterol, there’s no need to create a “forbidden list.”
Instead, think of certain foods as “sometimes choices” — items that can fit into a balanced diet but are best enjoyed in moderation, especially if you’re working to lower LDL and protect your heart.
The goal isn’t to remove enjoyment from eating.
It’s simply to understand which foods tend to push cholesterol levels upward and why.
High-Saturated-Fat Meats (Especially Fatty Cuts)
Red meats like fatty beef, lamb, bacon, and processed sausages can raise LDL.
This doesn’t mean you must give them up entirely — but choosing leaner cuts or enjoying them less often can make a noticeable difference.
A simple shift, like swapping two meat-based dinners per week for plant-based or fish-based meals, can be powerful.
Fried Foods & Fast Foods
Deep-fried meals often contain a combination of saturated and trans fats — both strongly linked to higher LDL and inflammation.
Even frying at home, though slightly better, still saturates foods with fats that your body struggles to process efficiently.
Choosing baked, sautéed, or grilled versions gives you the same flavor experience with far fewer consequences.
Highly Processed Snacks & Packaged Foods
Chips, packaged pastries, crackers, and certain convenience products may contain hydrogenated oils (a source of trans fats) or large amounts of refined carbohydrates.
These ingredients raise LDL and often increase triglycerides — a risky combination for heart health.
Look for snacks made from whole ingredients whenever possible.
Butter, Cream, and Full-Fat Dairy (in Excess)
Full-fat dairy products naturally contain saturated fat. While they can be part of a healthy diet, heavy use — especially in cooking or baking — can contribute to higher LDL levels.
Opting for moderate portions, lighter versions, or using olive oil more often helps create a healthy balance.
Refined Carbohydrates & Sugary Foods
White bread, pastries, sweets, and sugary drinks don’t directly raise LDL — but they do contribute to higher triglycerides, which can worsen overall cholesterol balance.
High sugar intake may even lower beneficial HDL.
Replacing some refined carbs with whole grains or fruit is a gentle way to support your heart.
Processed Meats (Salami, Hot Dogs, Deli Slices)
These foods combine saturated fat, sodium, and preservatives — a trio that’s hard on heart health.
They’re best kept as occasional treats rather than daily staples.
Why “Limit” Is More Realistic Than “Avoid”
Food should never feel like punishment. Heart health is built on consistency, not perfection. Even small weekly changes — fewer fried meals, more whole foods, lighter fats, smarter snacks — can significantly improve LDL and triglyceride levels over time.
In the next section, we’ll turn to one of the most powerful cholesterol-lowering tools of all: fiber, and how it works like a gentle internal sweep for your arteries.
Role of Fiber — How It Supports Cholesterol Balance
If there’s one nutritional hero in the journey toward lower cholesterol, it’s fiber — especially the soluble kind. Unlike trendy supplements or restrictive diet rules, fiber works quietly and reliably, supporting your heart in a way that feels almost effortless.
Most people don’t get enough of it, and yet it’s one of the simplest, gentlest tools your body uses to manage cholesterol every single day.
Soluble Fiber: The “Sponge” That Helps Remove LDL
Soluble fiber is found in foods like oats, beans, lentils, apples, berries, barley, and many vegetables.
When you eat it, it forms a soft, gel-like texture in your digestive tract. That gel literally binds to cholesterol particles and excess bile acids (which your body makes from cholesterol). Then, instead of sending them back into your bloodstream, your body simply gets rid of them.
The result is natural, gradual lowering of LDL — no drama, no complicated steps.
This is why people who add just one bowl of oats or a serving of beans a day often see real changes in a few weeks.
Insoluble Fiber: The Unsung Support System
Insoluble fiber doesn’t directly lower LDL, but it plays a supporting role by:
- keeping digestion regular
- helping stabilize blood sugar
- reducing overall inflammation
You’ll find it in whole grains, nuts, seeds, veggies, and wheat bran.
When your digestion runs smoothly and blood sugar is stable, cholesterol levels tend to follow.
Fiber Helps You Feel Full — Naturally
High-fiber foods slow digestion in a gentle, steady way.
This helps:
- prevent overeating
- stabilize appetite
- reduce cravings
- support healthy weight management
Since excess weight is closely linked with higher LDL and triglycerides, fiber indirectly protects your heart by promoting comfortable, natural fullness.
Fiber Supports a Healthier Gut — Which Supports Your Heart
A growing body of research shows that gut health and heart health are connected.
Fiber nourishes beneficial gut bacteria, which produce compounds that help:
- reduce inflammation
- support healthy blood vessels
- lower the risk of plaque buildup
A healthier gut often leads to healthier cholesterol levels.
How Much Fiber Do You Need?
Most adults need 25–30 grams a day, but many get half that amount.
The easiest way to increase it is simply to include more whole foods:
- a bowl of oats
- a serving of lentils
- an apple or orange
- a handful of nuts
- a colorful vegetable-filled dinner
Small steps add up quickly.
Fiber is one of the least restrictive, most supportive tools we have. No deprivation, no complicated planning — just nourishing, satisfying foods that work in harmony with your body.
Next, we’ll explore another key topic: healthy fats — and how choosing the right ones can dramatically shift your cholesterol profile for the better.
Healthy Fats vs. Harmful Fats — Choose the Right Oils
Fat isn’t the enemy — but the type of fat you choose can make all the difference for your cholesterol. This is one of the simplest areas of nutrition to adjust, and often one of the most rewarding. When you swap heavy, saturated fats for lighter, heart-friendly ones, your LDL begins to shift downward almost naturally, without feeling like you’re “on a diet.”
Let’s break it down gently and simply.
Why Some Fats Harm Your Heart
Saturated fats — the kind found in butter, fatty meats, full-fat dairy, and certain baked goods — tend to raise LDL cholesterol in the bloodstream. They’re not toxic or forbidden; they’re simply best treated as occasional guests on your plate rather than daily staples. Trans fats, found in partially hydrogenated oils, fried foods, and many processed snacks, are even more problematic because they raise LDL and lower HDL at the same time. This combination is especially hard on the arteries.
These fats aren’t always obvious. Sometimes they’re hiding in pastries, fast food, creamy sauces, or convenient packaged items. Becoming aware of where they show up is half the work — the other half is knowing what to use instead.
Healthy Fats That Support Cholesterol Balance
In contrast, monounsaturated and polyunsaturated fats help reduce “bad” LDL while supporting “good” HDL. They’re the kind of fats that your body recognizes easily and uses efficiently. Olive oil is the standout hero here — rich in antioxidants, beautifully anti-inflammatory, and a staple in many of the world’s longest-living cultures. Avocados, nuts, seeds, and oily fish (like salmon or mackerel) are also gentle powerhouses for your heart.
These fats don’t just help your cholesterol. They also bring flavor, satisfaction, and satiety — making meals feel complete and comforting, not restrictive.
Choosing the Right Oils in the Kitchen
A simple shift in cooking oils can change your cholesterol profile more than almost any other single habit. Using olive oil for sautéing, roasting, or dressing salads gives you a rich, smooth flavor and a meaningful heart-health boost. For high-heat cooking, avocado or grapeseed oil works well. If you enjoy butter, you don’t have to eliminate it — simply use it more sparingly and balance it with oils rich in monounsaturated fats.
Many people find that once they start experimenting with more flavorful oils, they naturally begin using less of the heavier options without trying.
Balance, Not Perfection
You don’t need to overhaul your entire diet to benefit. Small changes — swapping butter for olive oil a few times a week, adding avocado to lunch, using nuts instead of processed snacks — add up quickly. Over time, your arteries feel the difference.
Healthy fats aren’t about restriction; they’re about choosing options that work with your body rather than against it. And when your meals feel vibrant, flavorful, and satisfying, it becomes easy to nourish your heart every single day.
Eat the Rainbow — Fruits, Veggies & Antioxidants
One of the simplest, most enjoyable ways to lower cholesterol is also one of the most colorful. Fruits and vegetables aren’t just “healthy add-ons” — they are powerful, naturally protective foods that help your body manage cholesterol, support your arteries, and reduce inflammation. And the beautiful part is this: the more color you eat, the more your heart benefits.
Think of your meals as a canvas. Every shade — deep green, bright orange, ruby red, golden yellow, dark purple — represents a different set of antioxidants and plant compounds that gently support cholesterol balance.
Why Color Matters
Different pigments in fruits and vegetables represent different families of antioxidants. These antioxidants protect your arteries from oxidative stress — the process that turns LDL into something sticky and dangerous. That means the more color variety you include, the better your body can defend itself.
For example, deep purple foods like blueberries or red cabbage are rich in anthocyanins that help strengthen blood vessels. Orange produce like carrots and butternut squash contain beta-carotene, which supports overall heart function. Green vegetables like spinach, broccoli, and kale bring fiber, vitamins, and minerals that help regulate LDL and support healthy blood pressure.
Color isn’t just about beauty — it’s about biochemical diversity.
Fiber + Antioxidants = A Powerful Combination
Color doesn’t work alone. Fruits and vegetables are naturally high in fiber, especially soluble fiber, which binds to cholesterol and removes it from the body. When fiber and antioxidants show up together — as they do in most plant foods — they create a two-layer shield:
- Fiber lowers LDL by interrupting its reabsorption.
- Antioxidants prevent LDL from oxidizing and sticking to artery walls.
This is why even one colorful plate a day can generate measurable changes over time.
How to “Eat the Rainbow” Without Overthinking It
You don’t need complicated meal plans. Just try to add 2–3 different colors to each meal.
A morning bowl with berries, a lunch salad with greens and tomatoes, a dinner with sweet potatoes and broccoli — that’s already a rainbow day.
A small shift like replacing a beige snack (crackers, cookies, pastries) with something naturally colorful (an orange, sliced peppers, frozen berries, grapes) adds more antioxidants and fiber without any heaviness or restriction.
Fresh, Frozen, or Cooked? All Work.
Many people worry they “won’t get the full benefit” unless produce is raw and fresh. The truth is much simpler:
- Frozen fruit and vegetables often contain even more antioxidants.
- Cooked vegetables can make nutrients easier to absorb.
- Stews, soups, and roasted veggies remain incredibly heart-friendly.
In winter especially, warm, cooked dishes are not only comforting — they’re highly nutritious.
A Colorful Plate Helps Your Heart Feel Supported
Colorful meals feel energizing, vibrant, and satisfying. But they also send your body a clear message:
“I’m giving you what you need to protect me.”
And when fruits and vegetables become a natural part of your daily rhythm, cholesterol levels often respond quickly — sometimes even faster than people expect.
Sample Daily Meal Plan for Cholesterol Control
A heart-healthy eating pattern doesn’t need to feel like a diet. In fact, the best cholesterol-lowering meals are colorful, satisfying, and full of flavor. Below is a gentle, realistic one-day meal plan that shows what balanced eating can look like — nothing complicated, nothing extreme. Just simple, nourishing food choices that work with your body.
You can follow it closely, mix and match, or simply use it as inspiration to build your own version of a heart-supportive day.
🌅 Breakfast — Warm, Fiber-Rich, Energizing
Start your morning with something cozy that supports your cholesterol goals from the first bite.
Example:
A warm bowl of oatmeal made with rolled or steel-cut oats, topped with fresh or frozen berries, a sprinkle of chia or ground flaxseed, and a small handful of walnuts.
Why it works:
The soluble fiber in oats and berries works like a gentle sponge for LDL, while omega-3 fats from walnuts help lower inflammation and support HDL.
For a savory option:
Avocado toast on whole-grain bread with sliced tomatoes and a drizzle of olive oil.
☀️ Mid-Morning Snack — Light and Naturally Sweet
Choose something that keeps your energy steady without adding sugar spikes.
Example:
A crisp apple or orange paired with a few almonds.
Why it works:
Fruit provides antioxidants and fiber, and nuts offer healthy fats that support balanced cholesterol.
🍽️ Lunch — Colorful, Filling, Heart-Friendly
Keep lunch satisfying with a mix of lean protein, vegetables, and healthy fats.
Example:
A large salad bowl with mixed greens, chickpeas or lentils, chopped cucumber, tomatoes, shredded carrots, and a handful of quinoa. Top it with a simple olive-oil-and-lemon dressing.
Add sliced avocado or a spoonful of hummus for creaminess.
Why it works:
This meal is rich in soluble fiber, plant protein, and monounsaturated fats — the trio your heart loves most.
🌤 Afternoon Snack — Steady, Not Heavy
Rather than something sugary or processed, choose a snack that feels grounding.
Example:
Carrot sticks with hummus, or a small handful of pistachios.
Why it works:
Healthy fats + fiber = satisfied appetite and stable blood sugar.
🌙 Dinner — Warm, Balanced, and Nourishing
Dinner is a perfect time to include heart-supportive fats, fiber-rich sides, and antioxidant-packed vegetables.
Example:
Baked salmon (or trout) drizzled with olive oil and herbs, served with roasted Brussels sprouts and a side of quinoa or barley.
Why it works:
Omega-3s from fish reduce triglycerides, whole grains help lower LDL, and roasted veggies add fiber and antioxidants.
For a vegetarian option:
A lentil and vegetable stew cooked with tomatoes, onions, garlic, and leafy greens — deeply comforting and incredibly heart-friendly.
✨ Evening Treat — Something Gentle and Light
Yes, you can absolutely enjoy a treat while supporting cholesterol health.
Example:
A few squares of dark chocolate (70%+ cacao) or warm herbal tea with a slice of fruit.
Why it works:
Dark chocolate contains flavonoids that support blood vessels — small amounts go a long way.
The Philosophy Behind This Meal Plan
This day isn’t about perfection. It’s about balance:
- fiber at every meal
- healthy fats instead of heavy ones
- colorful produce
- lean proteins or plant proteins
- simple, satisfying flavors
Eating this way regularly can shift LDL downward, raise HDL, and leave you feeling lighter, clearer, and more energized.
Lifestyle Factors That Complement a Cholesterol-Lowering Diet
A heart-healthy diet is a powerful start — but when you pair it with supportive lifestyle habits, the benefits grow even stronger. Think of these habits as the “boosters” that help your body use nutrition more effectively. They’re not about radical change or intense routines; they’re about small, meaningful shifts that make your heart feel supported every day.
Here are the gentle lifestyle choices that work hand in hand with good food to naturally lower cholesterol and strengthen long-term cardiovascular health.
Move Your Body in Ways That Feel Good
Exercise helps increase HDL (“good” cholesterol) and encourages your body to clear LDL more efficiently. The best part? It doesn’t require a gym membership or intense workouts.
A daily walk, light stretching, yoga, cycling, dancing in your living room — it all counts. Even 20–30 minutes a day can improve cholesterol levels within weeks.
Consistency matters more than intensity.
Prioritize Good-Quality Sleep
Poor sleep can increase inflammation, raise LDL, and lower HDL — the opposite of what your heart needs.
Aiming for restful, consistent sleep supports healthy metabolism, better food choices, and more balanced cholesterol.
Small habits help: dim lights before bed, limit screens, keep your bedroom cool and quiet.
Manage Stress in Gentle, Realistic Ways
Stress hormones, especially cortisol, can raise cholesterol and blood pressure over time. You don’t need elaborate routines to feel calmer — even simple practices like five minutes of deep breathing, a warm cup of tea, a short walk, or journaling can soothe your nervous system.
The calmer your mind, the calmer your cardiovascular system.
Limit Alcohol and Quit Smoking (If Applicable)
Alcohol, especially in excess, raises triglycerides and can disrupt liver function — both strongly linked with higher cholesterol levels.
Smoking damages blood vessel walls and lowers HDL, making cholesterol more dangerous.
Cutting back on alcohol or eliminating smoking brings extraordinary benefits in a short time.
Maintain a Comfortable, Healthy Weight (If Needed)
Weight isn’t everything — but when extra weight sits around the abdomen, it often correlates with higher LDL and triglycerides.
The beauty is that you don’t need dramatic changes. Even losing 5–10% of your body weight (if recommended) can noticeably improve cholesterol numbers.
A balanced diet and gentle movement often lead to gradual, sustainable change.
Stay Hydrated & Limit Sugary Drinks
Adequate hydration helps your liver process fats more effectively.
Sugary drinks, on the other hand, spike triglycerides and contribute to insulin resistance — both major cholesterol disruptors.
Water, herbal tea, sparkling water with lemon — these make hydration feel refreshing and effortless.
Remember: It’s the Combination That Matters
No single lifestyle change carries the whole load.
But when they work together — a nourishing diet, steady movement, restful sleep, stress care — the effect becomes powerful, heart-protective, and lasting.
The goal isn’t a perfect routine. It’s a supportive rhythm that feels natural and sustainable for you.
FAQ — What People Really Ask About Diet and Cholesterol
Cholesterol is one of those topics that sparks a lot of confusion — and a lot of myths. People often leave the doctor’s office with numbers they don’t fully understand, or they read conflicting advice online and feel unsure about what actually helps. This FAQ gathers the most common, honest questions people ask and answers them in a simple, calm, human way.
No judgment, no complicated science — just clarity.
“Can I lower cholesterol without medication?”
Yes — for many people, diet and lifestyle changes can significantly lower LDL and triglycerides, especially when the levels are only moderately elevated. Foods rich in soluble fiber, healthy fats, antioxidants, and whole grains can create real improvements in as little as 4–12 weeks.
However, some people need medication due to genetics or medical history. Food is a powerful tool, but not always the only one — and that’s okay.
“Do I need to avoid fats completely?”
Not at all. Your body needs healthy fats for hormones, brain health, and energy. The key is choosing the right fats — olive oil, avocados, nuts, seeds, and fatty fish — while reducing heavy saturated fats and avoiding trans fats.
It’s about balance, not elimination.
“Is cholesterol from eggs dangerous?”
For most people, dietary cholesterol (like the cholesterol found in eggs) has much less impact on blood cholesterol than once believed. The bigger issue for cholesterol is saturated fat, not the cholesterol naturally present in whole foods.
Most people can enjoy eggs regularly as part of a heart-healthy diet.
“How fast can diet lower my cholesterol?”
Many people see changes in 4 to 12 weeks when they consistently follow heart-friendly habits. Soluble fiber, healthy fats, and omega-3s tend to bring the quickest improvements.
“Are plant-based diets the only way to lower cholesterol?”
No. Plant-based diets can be very effective, but they’re not the only path. Balanced diets that include fish, lean meats, whole grains, vegetables, fruits, and healthy fats can work beautifully.
The heart responds to patterns, not labels.
“Should I completely avoid cheese or dairy?”
Not necessarily. While full-fat dairy contains saturated fat, small or moderate portions can fit into a cholesterol-lowering diet — especially if balanced with vegetables, whole grains, and healthy fats.
Choosing lighter versions or using cheese as a flavorful accent rather than the main component works well.
“Do supplements help lower cholesterol?”
Certain supplements — like omega-3 fish oil, soluble fiber (psyllium), and plant sterols — can help, but they’re not magic fixes. Whole foods should always be the foundation, and supplements may be considered with guidance from a healthcare professional.
“If my cholesterol is high, do I have to give up all my favorite foods?”
Absolutely not. Most people succeed long-term by making gradual, realistic adjustments — not by eliminating everything they love.
Small swaps, better fats, more fiber, colorful produce, and mindful portions can create transformation without feeling like deprivation.
“Is high cholesterol always caused by diet?”
No. Genetics play a big role for many people. Even very healthy eaters can have elevated LDL due to hereditary factors. Diet is still incredibly helpful, but sometimes medication is part of the plan — and that is completely valid.